Translate this page into:
Orthodontic Clockwise Rotation of Maxillomandibular Complex for Improving Facial Profile in Late Teenagers with Class III Malocclusion: A Preliminary Report
Address for correspondence: Dr. Eric J. W. Liou, Department of Craniofacial Orthodontics, Chang Gung Memorial Hospital, 6F 199 Tung-Hwa North Road, 105, Taipei, Taiwan. E-mail: lioueric@ms19.hinet.net
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective
Orthodontic camouflage treatments improve occlusion but might worsen facial profile in patients with Class III malocclusion. It has been reported that surgical clockwise rotation of maxillomandibular complex (MMc) improves facial profile by reducing chin prominence and chin throat length in patients with Class III malocclusion. The purpose of this report was to illustrate two orthodontic techniques for clockwise rotation of the MMc in late teenagers with Class III malocclusion and preliminarily evaluate their clinical effects.
Patients and Methods
Six patients in late teenage with Class III malocclusion were included in this preliminary report. Bite raisers were first placed on the upper molars to open the bite and clockwise rotate the mandible. Intermaxillary elastics were then applied vertically between the upper and lower dentitions in 3 patients for bimaxillary extrusion (Technique-1) or between the upper dentition and the lower temporary anchorage devices (TADs) in another 3 patients (Technique-2) for upper dentition extrusion and closure of the anterior open bite. The three-dimensional cone-beam computed tomography images taken before and after orthodontic treatment were superimposed to evaluate the treatment effects of MMc clockwise rotation for both techniques.
Results
The Technique-1 extruded the upper and lower dentitions, rotated the mandible clockwise 2.01°, moved chin down 2.98 mm, and back −1.64 mm, although the mandible grew 2.47 mm during the treatment period. The Technique-2 extruded the upper dentition, rotated the mandible clockwise 0.90°, moved chin down 1.78 mm, but slightly forward 0.47 mm due to the mandible grew 2.50 mm and lower dentition was not extruded.
Conclusions
The orthodontic clockwise rotation of MMc is an effective technique for orthognathic camouflage. The applications of bite raisers and bimaxillary dentition extrusion could be more effective than single dentition extrusion with TADs in the mandible for clockwise rotation of MMc and improvement of occlusion and facial profile in late teenagers with Class III malocclusion. However, the comprehensive clinical effects and long-term stability need further clinical studies.
Keywords
Class III
maxillomandibular complex
orthognathics
camouflage
Introduction
The treatment of Class III malocclusion includes surgical orthodontics[1-4] or orthodontic camouflage treatment.[5-7] Orthodontic camouflage treatments, such as protraction of upper dentition and/or retraction of lower dentition through extraction or nonextraction therapy, improve the anterior crossbite in patients with Class III malocclusion.[8-11] The scope of Class III orthodontic camouflage treatment expands after the temporary anchorage devices (TADs) have been included.[9-11]
Orthodontic retraction of lower dentition also retracts lower lip and relatively worsens mandibular prognathism (excessive chin projection and chin throat length).[12] The goal of Class III orthodontic camouflage treatment should be an improvement of both occlusion and facial profile. However, mandibular prognathism are difficult to be camouflaged orthodontically.
Through orthognathic surgery, clockwise rotation of maxillomandibular complex (MMc)[13-15] has been proposed for a better improvement on mandibular prognathism, inadequate smile arc, and upper incisor show. An innovative concept and strategy of “orthodontic clockwise rotation of MMc” or “orthognathic camouflage” for patients with Class III malocclusion, therefore, has been developing.
Conceptually, the orthodontic clockwise rotation of MMc is opposite to the orthodontic counterclockwise rotation of MMc for patients with Class II anterior open bite. The contemporary orthodontic treatment for patients with Class II anterior open bite is to intrude the upper/ lower posterior teeth and counterclockwise rotate mandible for closing anterior open bite and improving mandibular retrognathism (inadequate chin projection and short chin throat length).[16,17] On the contrast, the orthodontic clockwise rotation of MMc is to extrude the upper dentition for improving upper incisors show and smile arc, and subsequently to clockwise rotate the mandible for improving mandibular prognathism in either growing or nongrowing patients. The strategy is to place bite raisers/blocks on posterior teeth to open the bite and clockwise rotate the mandible backward and downward to the planned position, and then the anterior open bite is closed by extrusion of the upper dentition.
The purpose of this report was to illustrate two orthodontic techniques for clockwise rotation of MMc and preliminarily evaluate their clinical effects in late teenagers with Class III malocclusion.
Patients and Methods
Six patients with Class III malocclusion in late teenage were included in this preliminary report, including 3 patients treated by orthodontic clockwise rotation of MMc without TADs [Technique-1, Figures 1 and 2], and another 3 patients treated by orthodontic clockwise rotation of MMc with TADs in the mandible [Technique-2, Figures 3 and 4].

- The clinical procedure and case report of the Technique-1 for orthodontic clockwise rotation of maxillomandibular complex in a 15-year-old female teenager with Class III malocclusion. (a) The pretreatment extraoral and intraoral photographs; (b) Placement of bite raisers on upper posterior teeth and application of anterior vertical elastics for bimaxillary extrusion of anterior teeth and premolars after the upper the and lower dentitions were aligned and expanded; (c) Removal of bite raisers and application of a maxillary continuous posterior teeth extruding lever arch together with anterior intermaxillary vertical elastics for maxillary posterior teeth extrusion after 5 months of clockwise and stepwise rotation of maxillomandibular complex; (d) Placement of a continuous maxillary archwire for alignment and leveling after 5 months maxillary posterior teeth extrusion; (e) The posttreatment extraoral and intraoral photos
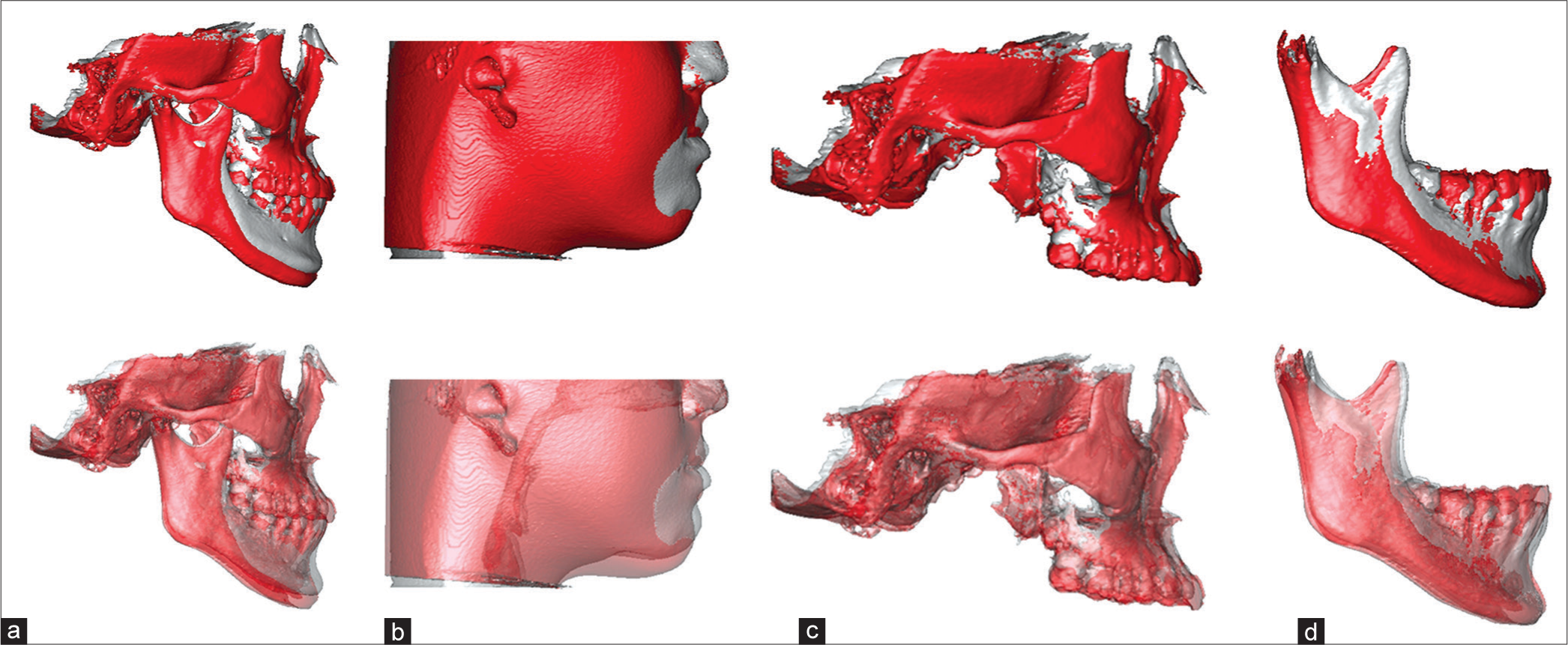
- The three-dimensional superimpositions of the pretreatment (silver-gray color) and posttreatment (red color) cone-beam computer tomography images of the Technique-1 case report in Figure 1. (a) The overall skeletal superimposition on cranial base revealed the mandible was clockwise rotated 2.9°, downward 5.5 mm, and backward 3.2 mm; (b) The overall soft-tissue superimposition based on overall skeletal superimposition on cranial base revealed the soft-tissue chin project was reduced 3.4 mm; (c) The cranial base superimposition without mandible revealed the maxillary dentition was extruded 2.5-4.3 mm; (d) The mandibular superimposition illustrated the lower dentition was extruded 1.8–5.5 mm, and the mandible grew 3.3 mm

- The clinical procedure and case report of the Technique-2 for orthodontic clockwise rotation of maxillomandibular complex in a 16.4-year-old male teenager with Class III malocclusion. (a) The pretreatment extraoral and intraoral photographs; (b) Placement of bite raisers on upper posterior teeth and application of anterior vertical elastics between upper anterior teeth and lower temporary anchorage devices for the extrusion of upper dentition, and intrusion of lower dentition with lower temporary anchorage devices; (c) Removal of bite raisers and application of a maxillary continuous posterior teeth extruding lever arch together with anterior vertical elastics for maxillary posterior teeth extrusion after 13 months of clockwise and stepwise rotation of maxillomandibular complex; (d) Placement of a continuous maxillary archwire and Class III elastics after 6 months of maxillary posterior teeth extrusion; (e) The posttreatment extraoral and intraoral photos
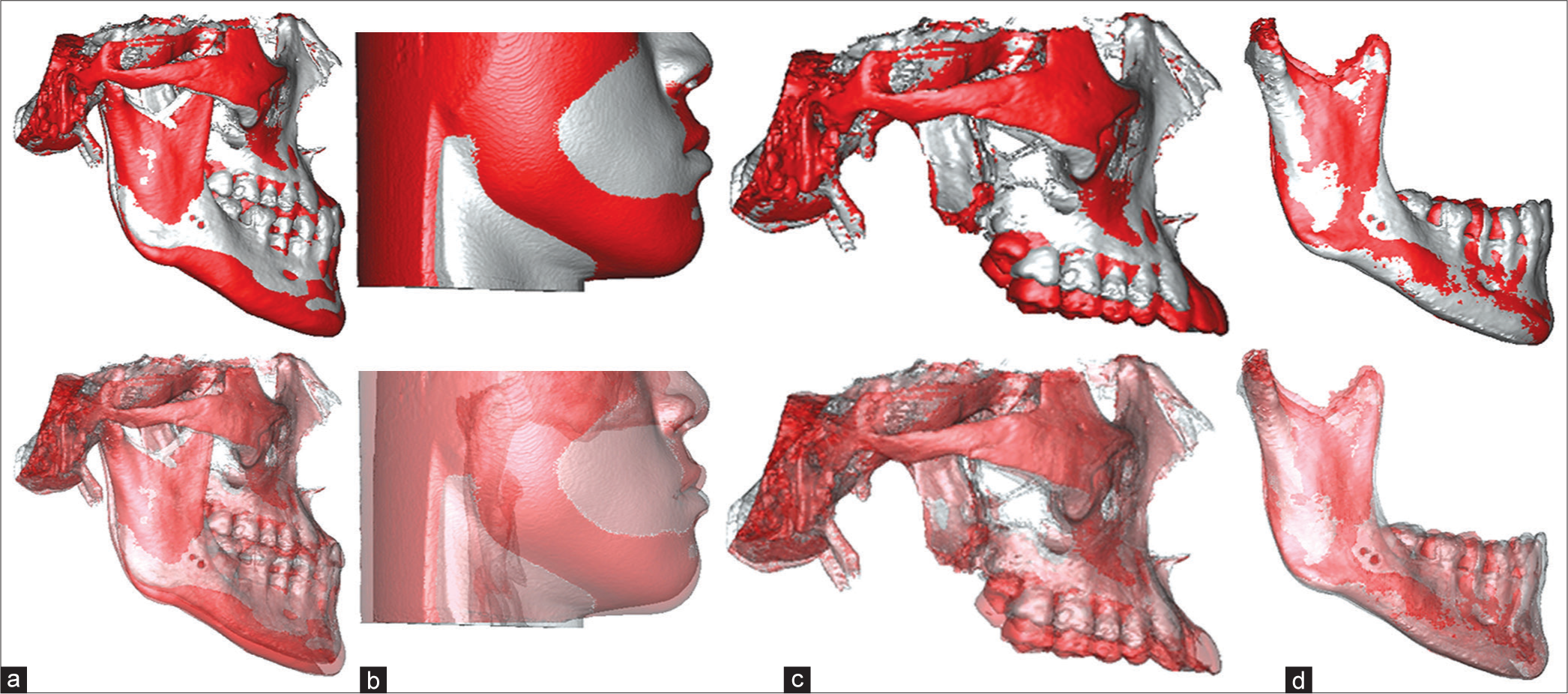
- The three-dimensional superimpositions of the pretreatment (silver-gray color) and posttreatment (red color) cone-beam computer tomography images of the Technique-2 case report in Figure 3. (a) The overall skeletal superimposition on cranial base revealed the mandible was clockwise rotated 0.9°, downward 3.7 mm, but forward 1.5 mm; (b) The overall soft-tissue superimposition based on overall skeletal superimposition on cranial base revealed the soft-tissue chin moved downward 4.5 mm but forward 1.3 mm due to inadequate clockwise rotation of mandible, growth of mandible, and no extrusion of lower dentition; (c) The cranial base superimposition without mandible revealed the maxillary dentition was extruded 0.9–6.6 mm; (d) The mandibular superimposition illustrated lower dentition was intruded 1.1–2.7 mm, and the mandibular condyle grew 3.7 mm
Technique-1
Preparation
A segmental maxillary archwire from second premolar to second premolar with anterior labial crown torque was placed, and another two segmental archwires were placed on both sides of the maxillary first and second molars. A transpalatal arch (TPA) was placed to consolidate the maxillary posterior teeth. A continuous archwire and a lingual holding arch (LHA) were placed in the mandibular dentition.
Placement of bite raisers
The material for bite raisers could be light-cured composited resin or glass ionomer (GI) band cement. For the ease of saliva control, bonding, and removal, bonding light-cured GI band cement on the upper posterior teeth is recommended.
The occlusal surfaces of upper molars on both sides were cleaned with pumice powder, and then, the central fossae of the molars but not the entire occlusal surface were etched with etching agent. The etching process at the central fossae ensured retention of the bite raisers without dislodgement during the treatment and ease of removal after the treatment. The GI band cement was then added incrementally on the occlusal surfaces of the upper molars until 2–3 mm bite opening at the anterior teeth.
Extrusion of anterior teeth
After the bite raisers were placed, intermaxillary vertical elastics between the upper and lower anterior teeth were then applied for extruding the upper dentition. Patients were instructed to wear the intermaxillary vertical elastics 14–20 h/day and arranged back in clinic on monthly schedule. The increment of GI band cement was added to keep the bite opened 2–3 mm at each visit so that the mandible rotated clockwise and stepwise every month.
Extrusion of posterior teeth
After the upper anterior teeth occluded with lower dentition and the mandible had clockwise and stepwise rotated to the planned position, the bite raisers were then removed and a maxillary continuous posterior teeth extruding lever arch together with anterior intermaxillary vertical elastics was placed for maxillary posterior teeth extrusion, or simply applied intermaxillary posterior vertical elastics for extruding the upper and lower molars. Buccal crown torque or lateral expansion was then added to the TPA and LHA for avoiding palatal or lingual tipping during extrusion of molars.
After the upper and lower posterior teeth had occluded, a continuous maxillary archwire was then placed to replace the segmental archwires in the maxillary dentition.
Technique-2
Preparation and insertion of temporary anchorage devices
The preparation was the same as the Technique-1. To rotate the mandible without extruding the lower dentition, TADs were placed in the anterior of the mandible. The TADs could be inserted interdentally between the mandibular canine and premolar on both sides.
Placement of bite raisers and extrusion of upper anterior teeth
The placement of the bite raisers was the same as the Technique-1. After insertion of the TADs in mandible and placement of bite raisers on the occlusal surfaces of maxillary posterior teeth, intermaxillary vertical elastics were then applied between the upper anterior teeth and the lower TADs for extruding the upper dentition.
Extrusion of posterior teeth
After the upper anterior teeth occluded with lower dentition and the mandible had clockwise and stepwise rotated to the planned position, the bite raisers were then removed and a maxillary continuous posterior teeth extruding lever arch together with anterior intermaxillary vertical elastics was placed for maxillary posterior teeth extrusion, or simply applied intermaxillary posterior vertical elastics for extruding the upper and lower molars. Buccal crown torque or lateral expansion was added on the TPA and LHA for avoiding palatal or lingual tipping during extrusion of molars.
After the upper and lower posterior teeth had occluded, a continuous maxillary archwire was then placed to replace the segmental archwires in the maxillary dentition.
All the patients had pretreatment (T0) and posttreatment (T1) cone-beam computed tomography (CBCT). The CBCT images at T0 and T1 were superimposed on the cranial base for the vertical changes of upper anterior/posterior teeth, positional changes of mandible at menton (Me) and pogonion (Pog), and mandibular plane angle; they were also superimposed on the mandibular symphysis, mental foramina, inferior alveolar canals, and inferior borders of mandible for the vertical changes of lower anterior and posterior teeth, and changes of mandibular length (Co-Pog) [Figures 2 and 4]. All the superimpositions and measurements were performed under SimPlant O&O (Materialise, Belgium).
Results
The average age was 15.8 years at T0 and 17.9 years at T1 for the Technique-1 group and was 16.3 years at T0 and 18.6 years at T1 for the Technique-2 group. The average treatment period (T1–T0) was 2.1 years for the Technique-1 group and 2.3 years for the Technique-2 group. Both Technique-1 and 2 rotated the mandible clockwise [Figures 2 and 4].
The Technique-1 extruded the upper and lower dentitions, rotated the mandible clockwise 2.01°, moved chin down 2.98 mm and back − 1.64 mm, although the mandible grew 2.47 mm at T1–T0. The Technique-2 extruded the upper dentition, rotated the mandible clockwise 0.90°, moved chin down 1.78 mm but slightly forward 0.47 mm, due to the mandible grew 2.50 mm at T1–T0 and lower dentition were not extruded [Table 1].
| T1-T0 | UI-Ext (mm) | UM-Ext (mm) | LI-Ext (mm) | LM-Ext (mm) | MP (°) | Me-down (mm) | Pog-back (mm) | Md-growth (mm) |
|---|---|---|---|---|---|---|---|---|
| Technique-1 | 2.96±0.39 | 3.61±1.19 | 2.98±2.42 | 2.18±0.53 | 2.01±0.76 | 2.98±2.25 | −1.64±2.31 | 2.47±2.01 |
| Technique-2 | 1.05±1.41 | 4.76±2.36 | 0.63±3.83 | −1.47±0.89 | 0.90±0.45 | 1.78±1.70 | 0.47±1.00 | 2.50±1.15 |
Negative value – Intrusion or backward movement; UI-Ext – Upper incisor extrusion; UM-Ext – Upper molar extrusion; LI-Ext – Lower incisor extrusion; LM-Ext – Lower molar extrusion; MP – Mandibular plane angle; Me-down – Menton downward movement; Pog-back – Pogonion backward movement; Md-growth – Mandibular growth
Discussion
Orthodontic clockwise rotation of MMc for improving mandibular prognathism in patients with Class III malocclusion has not been reported before. It includes extrusion of maxillary dentition and clockwise rotation of mandible. This technique could be used in either nonextraction or extraction, growing or adult patients.
Maxillary hypoplasia and/or mandibular prognathism are the most two common features in patients with Class III malocclusion. The maxillary hypoplasia includes sagittal and/or vertical deficiency. Unfortunately, the Class III orthodontic camouflage treatment usually focuses on the sagittal improvement of anterior cross bite[5-7] but seldom on the improvement of maxillary vertical deficiency.
Orthodontic extrusion or force eruption has been used successfully for implant site development to augment alveolar vertical bone height.[18-20] Similarly, both the Technique-1 and 2 in this report extruded the maxillary dentition 1–4 mm. We inferred the extrusion of maxillary dentition developed the maxillary alveolar vertical bone height and subsequently improved the maxillary incisors show and smile arc, clockwise rotated the mandible, reduced chin prominence, and shortened the chin throat length. This is a concept of “orthognathic camouflage” for mandibular prognathism without surgical reduction of mandibular length.
The Technique-1 rotated the mandible downward and backward, but the Technique-2 rotated the mandible downward. This could be due to the mandible grew 2.47–2.50 mm during the treatment period, and the extrusion mechanism was bimaxillary in the Technique-1 but only single dentition in the Technique-2. In addition to the extrusion of maxillary dentition, the extrusion of lower dentition further clockwise rotated the mandible backward and downward. It is, therefore, the Technique-1 could be more effective than the Technique-2 to clockwise rotate the mandible downward and backward. The Technique-2 might spend more time in rotating the mandible clockwise without extrusion of the lower incisors. However, the Technique-1 extruded the lower incisors and unfavorably increased lower incisor show during smile. For patients with excessive lower incisor show, the Technique-2 is indicated rather than the Technique-1.
The extrusion of maxillary or mandibular dentition was a two-step procedure. The dentition before the second premolars was extruded first then the molars due to the bite raisers were placed on molars. Bite raisers opened the bite but also intruded molars in certain amount when patient bites. This certain amount of molar intrusion might compromise and slow down the process of clockwise rotation of mandible, although our results revealed the upper molars were well extruded at the end of treatment. The bite raisers could be placed on maxillary second molars in the first few months and then alternatively be placed on the maxillary first molars to diverse the effects of molar intrusion by biting force.
Clockwise rotation of MMc also increases anterior facial height and might lead to lip incompetence. It is therefore clockwise rotation of MMc should be stopped before the development of lip incompetence. Orthodontic clockwise rotation of MMc is best indicted for Class III patients with short face, low angle, maxillary vertical deficiency, or overclosure, and it might not be indicated for Class III patients with long face, high angle, open bite, or lip incompetence. Class III patients with lip incompetence due to dentoalveolar protrusion could still be indicated through extraction therapy.
Although the long-term stability of orthodontic extrusion has not well revealed yet, the 1–3 years posttreatment results were reported stable in some case reports.[21-23] On the contrast, the stability of orthodontic intrusion has been documented and the 3–4 years posttreatment relapse of orthodontic intrusion of posterior teeth was 13.37% to 22.88%.[24,25] We hypothesized the long-term stability of orthodontic extrusion could be similar to that of orthodontic intrusion, and overcorrection is commended for the clockwise rotation of MMc in patients with Class III malocclusion.
Conclusions
The orthodontic clockwise rotation of MMc is an effective technique for orthognathic camouflage. The applications of bite raisers and bimaxillary dentition extrusion could be more effective than single dentition extrusion with TADs in the mandible for clockwise rotation of MMc and improvement of occlusion and facial profile in late teenagers with Class III malocclusion. However, the comprehensive clinical effects and long-term stability need further clinical studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The surgical tools: The leFort I, bilateral sagittal split osteotomy of the mandible, and the osseous genioplasty. Clin Plast Surg. 2007;34:447-75.
- [CrossRef] [PubMed] [Google Scholar]
- The history of the “Le fort I osteotomy”. J Maxillofac Surg. 1986;14:119-22.
- [CrossRef] [Google Scholar]
- Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35:157-9.
- [Google Scholar]
- Multiple-segment osteotomy in maxillofacial surgery. Plast Reconstr Surg. 1999;104:381-8.
- [Google Scholar]
- Limitations in orthopedic and camouflage treatment for class III malocclusion. Semin Orthod. 2007;13:158-74.
- [CrossRef] [Google Scholar]
- Class III camouflage treatment: What are the limits? Am J Orthod Dentofacial Orthop. 2010;137:9.e1-9.e13.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontic camouflage in skeletal class III malocclusion: A contemporary review. J Orofac Res. 2014;4:98-102.
- [Google Scholar]
- Camouflage treatment in adult skeletal class III cases by extraction of two lower premolars. Korean J Orthod. 2010;40:349-57.
- [CrossRef] [Google Scholar]
- Class III malocclusion with complex problems of lateral open bite and severe crowding successfully treated with miniscrew anchorage and lingual orthodontic brackets. Am J Orthod Dentofacial Orthop. 2011;139:679-89.
- [Google Scholar]
- Camouflage treatment of skeletal class III malocclusion with multiloop edgewise arch wire and modified class III elastics by maxillary mini-implant anchorage. Angle Orthod. 2013;83:630-40.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of treatment outcomes between temporary anchorage devices and class III elastics in class III malocclusions. Am J Orthod Dentofacial Orthop. 2017;151:1116-24.
- [Google Scholar]
- The influence of lower lip position on the perceived attractiveness of chin prominence. Angle Orthod. 2013;83:795-800.
- [CrossRef] [PubMed] [Google Scholar]
- Correction of skeletal class III malocclusion with clockwise rotation of the maxillomandibular complex. Am J Orthod Dentofacial Orthop. 2012;141:219-27.
- [Google Scholar]
- Rotation of the maxillomandibular complex to enhance esthetics using a “surgery first” approach. J Clin Orthod. 2012;46:85-91.
- [Google Scholar]
- Posterior pharyngeal airway in clockwise rotation of maxillomandibular complex using surgery-first orthognathic approach. Plast Reconstr Surg Glob Open. 2015;3:e485.
- [CrossRef] [PubMed] [Google Scholar]
- Management of acquired open bite associated with temporomandibular joint osteoarthritis using miniscrew anchorage. Korean J Orthod. 2012;42:144-54.
- [Google Scholar]
- Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: A systematic review. Prog Orthod. 2016;17:9.
- [Google Scholar]
- The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13:312-33.
- [CrossRef] [Google Scholar]
- Implant site development by orthodontic forced eruption of nontreatable teeth: A case report. Open Dent J. 2012;6:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of slow forced eruption on the vertical levels of the interproximal bone and papilla and the width of the alveolar ridge. Korean J Orthod. 2016;46:379-85.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical approach to class I open-bite malocclusion with extrusion mechanics: A 3-year retention case report. Am J Orthod Dentofacial Orthop. 2015;147:499-508.
- [Google Scholar]
- Cephalometric evaluation of open bite treatment with Niti arch wires and anterior elastics. Am J Orthod Dentofacial Orthop. 1999;116:555-62.
- [Google Scholar]
- Effect of presurgical incisor extrusion on stability of anterior open bite malocclusion treated with orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1998;13:23-34.
- [Google Scholar]
- Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010;138(396):e1-9.
- [Google Scholar]
- Evaluation of long-term stability of skeletal anterior open bite correction in adults treated with maxillary posterior segment intrusion using zygomatic miniplates. Am J Orthod Dentofacial Orthop. 2016;150:78-88.
- [CrossRef] [PubMed] [Google Scholar]






